Cauda Equina Syndrome
Cauda equina syndrome (CES) requires rapid recognition and emergent decompression for optimal bladder, bowel, and motor outcomes. Diagnostic clarity can be clouded by overflow incontinence, analgesic use, and communication barriers; vigilance is paramount.
Clinical Criteria and Pitfalls
- Red flags: urinary retention, saddle anesthesia, bilateral sciatica, progressive bilateral weakness, fecal incontinence.
- Examine: post-void residual by bladder scan, anal tone, perianal sensation; document carefully.
- Do not miss: severe central disc herniation, epidural abscess/hematoma, tumor, or fracture-retropulsion.
Imaging Examples

CES due to posterior epidural abscess. Source: Wikimedia Commons (CC BY 4.0; © Chan & Oh).

Large L4-L5 paramedian disc can precipitate CES if massive and central. Source: Wikimedia Commons (CC0).

Animated T2 overview to contextualize multilevel degeneration. Source: Wikimedia Commons.
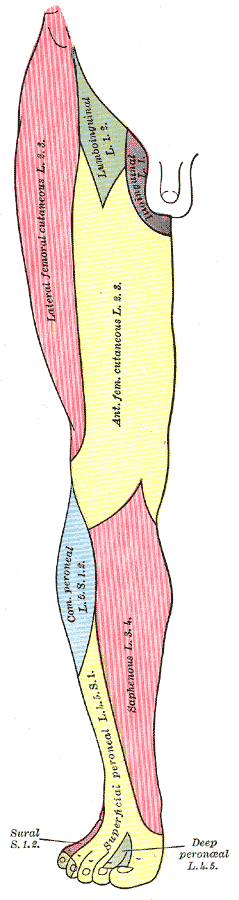
Dermatomal reference for correlating sensory loss. Source: Wikimedia Commons (Public Domain).
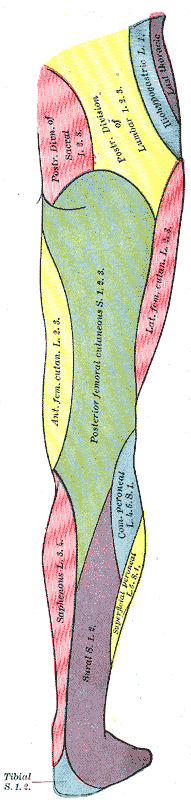
Posterior dermatomes highlighting sacral segments relevant to perineal sensation. Source: Wikimedia Commons (Public Domain).

Nerve map aid for lower motor neuron pattern recognition. Source: Wikimedia Commons (Public Domain).

Severe central stenosis can predispose to acute neurologic deterioration with superimposed disc or hematoma. Source: Wikimedia Commons (CC BY-SA 3.0).
Management and Timing
- Emergent MRI and urgent decompression when CES suspected; do not delay for full labs unless sepsis suspected.
- Broad-spectrum antibiotics prior to decompression if abscess; urgent drainage.
- Document pre-op neurologic and bladder status; early catheterization for retention with post-op weaning plan.
Postoperative Course and Medico-legal Notes
- Earlier surgery correlates with improved bladder outcomes; residual deficits common when presentation is delayed.
- Maintain clear documentation of timing, counseling, and examination findings.
You can contact us at @bdthombre(https://www.linkedin.com/in/bdthombre/ ) on LinkedIn.